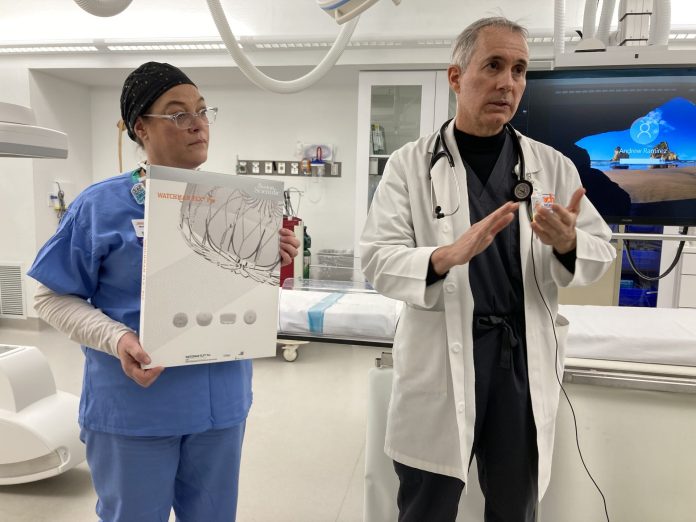
Medical Center Hospital is now the only facility in the Permian Basin to offer the updated WATCHMAN FLX Pro Device as part of an alternative procedure for people with atrial fibrillation not caused by a heart valve problem.
Dr. Fernando Boccalandro, an interventional cardiologist and medical director for the cardiovascular services at MCH, said the hospital has been placing WATCHMANs for four years, but this is a new generation of the device.
The WATCHMAN device is a novel alternative for patients with non-valvular atrial fibrillation at risk for stroke, especially those with a compelling reason not to be on blood thinners. The device closes off an area of the heart called the left atrial appendage to keep harmful blood clots that can form in the left atrial appendage from entering the blood stream and potentially causing a stroke.
“It’s a new device that is optimized compared with the prior devices, so it has several technical features that are better than the old devices so it allows you to place the device with more ease. (There are) some markers in the device that allow you to visualize it better on the X ray. Also it is covered by a new coat called HEMOCOAT, which is a cover in the fabric of the device which is much more biocompatible than the prior generation of the devices and also comes in a bigger size,” allowing doctors to put it in a wider patient population, Boccalandro said.
He added that atrial fibrillation is a very common rhythm.
“Approximately 5 million people in the U.S. have atrial fibrillation aythnia and a lot of these people that have this are required to be on blood thinners for stroke prevention. Of this group, there is a subgroup of patients that have difficulty taking blood thinners because they have higher bleeding risk, either because they have bled or have fall(en) and it’s felt that the blood thinners will be risky for them to take over a lifetime,” Boccalandro said.
He added that this is the only intervention that they can do to decrease the risk of stroke and bleeding without the use of blood thinners in the long term.
The device goes in a pouch that everyone has in the left atrium. Boccalandro and Drs. Manohar Angirekula and Adam Farber have performed more than 150 of these procedures at Medical Center with excellent outcomes and are looking forward to improving the outcomes with the new device. Michelle Judy, the structural heart coordinator, is also an integral part of the team.
“It’s a little like a wind sock that we all have in common. The first thing that we do is before the procedure we actually measure the dimensions of that pocket to make sure that the size of the device will be appropriate for individual patients and then the day of the procedure we will bring the patient to the cath lab … Then under general anesthesia and an ultrasound that allows to maneuver inside the heart, we make a small puncture in the groin area. From there, we can selectively place the device in the pouch, and then we verify and ensure the device is in the correct location and that pouch is sealed. And then we can just close a small hole that we make. It’s a very, very small hole. Most of the patients stay overnight in the hospital for observation and then they can go home,” Boccalandro said.
The procedure takes about an hour to perform and is minimally invasive, he added. The patient can go home the day after the procedure and it takes two or three days to get back to normal.
“What it does is it mechanically seals that pouch. It will be almost like putting a cork right in a bottle, so we are able to seal that with the device itself. The device has a fabric, so we’re able to seal the pouch completely with the fabric of the device,” Boccalandro said.
Once implanted, the objective is for the device to stay in for the lifetime of the patient.
“We don’t have to replace the device. We don’t have to do any maintenance of the device. We do recheck the device … 45 days to 90 days after the device is implanted …,” with an ultrasound to make sure it is in a good position and working well, Boccalandro said.
He noted that the device doesn’t truly change the rhythm of the heart, but it prevents the formation of blood clots in the pouch because the pouch is now filled with the device so “you don’t have space to be able to form a block.”
They check to see if there is a blood clot forming or already there before they put the device in. If there is, they don’t try to put it in.
“In those cases, we usually treat the patient with blood thinners for approximately four to six weeks and that tends to dissolve the majority of the blood clots. During the procedure, however, to prevent any blood clot formation when we’re working on manipulating the heart, we maintain the patient on a predictable blood thinner that we measure throughout the procedure to make sure that the blood is thin enough that the patient cannot form a blood clot during the procedure. But if you already have a blood clot in the pouch, we have to wait until that block is dissolved,” Boccalandro said.
Checkups are done at 45 to 90 days with an ultrasound.
“It’s noninvasive. It’s just coming to the hospital to do an ultrasound, or something we can do a CAT scan as well. That’s the only thing that we need to check after an implant. Other than that, there’s no other checkup we need,” Boccalandro said.
He added that this is an excellent service that they provide in the Permian Basin.
“There’s a lot of technology currently involved to try to optimize the whole procedure to try to make it easier. … It’s a good possibility that in the future, this will be the first-line therapy,” Boccalandro said.
This is the third-generation WATCHMAN and there is a big difference between the first and second generations in terms of safety, he said.
Like every other technology, Boccalandro said, it gets better every day.
“We’re just going to see how the next generation of devices are going to be even better than what we have today,” he added.



